COVID 19: Surface Cleaning and Disinfection
The purpose of this document is to present the current knowledge on cleaning and disinfecting surfaces in indoor and outdoor environments, specifically in residential settings and public spaces and excluding healthcare facilities and other healthcare settings, as well as on health issues related to cleaners and disinfectants and the suggested “quarantining” of objects. The information summarized in this document is based on a non-comprehensive review of the grey and scientific literature. The sections in yellow are significant updates made on the indicated date, based on the grey literature available as at April 26, 2021. Complete information on the methodology used to create this document is presented in Appendix 1.
Persistence of the SARS-CoV-2 virus on surfaces and fomite transmission
Detection and persistence of the virus on surfaces and inanimate objects
In real conditions, the SARS‑CoV‑2 virus, or its genetic material (RNA), have been detected on surfaces in a number of studies conducted in healthcare settings (3–22) and in the community (14,23–28). It is generally reported that the environment is most contaminated near infected individuals and on the surfaces they frequently touch (4–6,23). However, no research teams have been able to cultivate the virus when present on surfaces in non-experimental settings (5,9,13,19,24,29).
Depending on the surfaces examined, different authors have reported a varying duration from a few hours to a few days in which the virus was cultivable in experimental conditions. The duration was longer on stainless steel (48 hours) and plastic (72 hours), and shorter on cardboard (24 hours) and copper (4 hours) (30). Chin et al. (2020) have reported detecting the virus for a period of up to three hours following inoculation on rougher surfaces like paper and fabric, and seven days on smooth surfaces like plastic and steel (31). The virus remained cultivable for less than 24 hours on bank notes and clothing (32). Liu et al. (2020) have reported that SARS‑CoV‑2 remained cultivable for seven days on plastic, stainless steel, glass, ceramic, wood, latex gloves, and surgical masks, but that no virus could be cultivated from cotton clothing after four days or from paper after five days (33). The virus therefore generally appears to survive longer on smooth surfaces than on porous surfaces in a lab (31,33). It is important to note that the experimental conditions recommended by the previously cited authors are most often more favourable to the persistence of the virus than field conditions, which did not allow for cultivation of the virus.
Preservation of the virus on surfaces depends on a number of factors including environmental conditions like temperature and relative humidity. In outdoor environments, preservation is generally affected by wind speed, precipitation, and the intensity of ultraviolet (UV) rays (34). With regard to UV rays, laboratory experiments have indicated that the SARS‑CoV‑2 virus has a very quick inactivation rate in aerosols in sunlight, with a half-life of less than six minutes and 90% of the virus inactivated within 20 minutes at varied sunlight intensities (35). UVC radiation has also been demonstrated as effective at inactivating SARS‑CoV‑2 in a virus suspension (36).
Virus transmission through contact with surfaces and inanimate objects
To date, few epidemiological studies have shown that COVID‑19 can be transmitted via fomites (37–41). The specifications required to demonstrate this link are complex, especially since it is difficult to fully exclude other possible means of transmission. One experimental study on hamsters established that SARS‑CoV‑2 can be transmitted between these animals via contaminated surfaces (42). While no clear human transmission specifically attributable to contact with fomites has been identified in the literature, the World Health Organization (WHO) (43–45) and a number of scientific literature reviews (46–50) have concluded that this form of transmission remains possible. The Centers for Disease Control and Prevention (CDC) consider the risk of SARS-CoV-2 transmission via fomites to be low (51).
Prevention and control measures
The prevention and control measures generally recommended in a pandemic context, such as minimizing contacts, physical distancing, hand hygiene, use of respiratory etiquette, and mask-wearing are considered essential for reducing the risk of contracting SARS‑CoV‑2. Also, cleaning is facilitated by limiting clutter and removing non-essential objects that are difficult to clean (52).
Cleaning and disinfection
- Wet cleaning methods (e.g., with a clean, damp cloth or wet mop) are preferable to dry methods (dusting and sweeping), as they are less likely to resuspend infectious aerosols in the air (1).
- The cleaners and disinfectants commonly found on the market and approved by Health Canada are effective against the virus that causes COVID-191(53,54).
- It is important to always follow the manufacturer’s instructions for using these products and not to mix different products, as such solutions can generate irritating and noxious fumes. It is also important to ensure that the product is in contact with the surface to be disinfected for a sufficient amount of time. This contact time is usually specified by the product manufacturer (55).
- The most frequently touched surfaces (door handles, armrests, tables, light switches, remote controls for electronic equipment, water faucets, elevator buttons, handrails, toilets, etc.) are more likely to be contaminated by SARS-CoV-2. Particular attention must be paid to the frequency and rigorous effectiveness of their cleaning and disinfection, as needed.
- For porous surfaces such as carpets and curtains, any visible contamination, when present, must be eliminated using suitable cleaning products specified for use on these surfaces. After cleaning, if the articles can be washed, it is recommended to do so in accordance with the manufacturers’ instructions using the maximum water temperature recommended for these articles, if possible (1,56), and to then dry them completely afterwards.
Health problems associated with cleaning products and disinfectants
Between March and June 2020, there was a significant increase in telephone calls to Canadian poison control centres regarding exposure to disinfectants for surfaces and hands (e.g., bleach, chlorine/chloramine gas) compared to the same period in 2019. The rapid increase in calls in the third week of March 2020 coincides with the WHO declaring the international pandemic and is consistent with results gathered in the United States (57). Data collected from 55 American poison control centres also showed a significant increase in calls (20.4%) regarding cleaning products and disinfectants from January to March 2020, compared to the same period in 2019, with the number of cases primarily increasing in March 2020. Diluted bleach solutions (62.1%) and alcohol-free hand sanitizers (36.7%) were the main causes of this increase. Cases of inhalation exposure particularly increased, both for cleaning products (35.3%) and for all disinfectants (108.8%) (58).
A recent study, also from the United States, may partly explain these increases. A survey of citizens’ knowledge and behaviours regarding cleaning and disinfection related to the COVID-19 pandemic showed that a third of respondents reported risk behaviours, such as cleaning food products with bleach, applying disinfectants to skin that were not designed for this use, or inhaling or even intentionally ingesting cleaning products or disinfectants. The authors concluded that there is a need to inform citizens about safe cleaning and disinfection practices (59).
The use, and particularly the inappropriate use, of cleaning products and disinfectants can cause acute health problems. A notable example is mixing bleach with other ammonia- or acid-based products. In the former case, the mixture can produce chloramine gases that may cause respiratory effects in persons exposed, including shortness of breath, wheezing, and irritation of the eyes, throat, and nose, etc. In the latter, chlorine gas can be produced, with equally harmful respiratory consequences (60).
Regarding possible chronic health problems, epidemiological data have shown an association between the use of cleaning products and disinfectants in the workplace (61) and at home (62,63) with the development and exacerbation of asthma. An international study has also established a relationship between the use of household cleaning sprays and the incidence of adult asthma (62).
Cleaning and disinfecting frequently touched objects and surfaces (see Method for cleaning and disinfection), as needed, are recommended and necessary prevention and control measures in the fight against COVID-19. However, considering the increase in acute effects related to exposure to cleaning products and disinfectants observed in Canada (57) and the United States (58) in the spring of 2020 and that possible inappropriate use of these products has been demonstrated (59), there is good reason to emphasize their safe use. In particular, it is important to follow the manufacturers’ instructions and to avoid mixing products (see Prevention and control measures – Cleaning and disinfection; third point), to respect protective measures (see Appropriate protective measures for cleaning and disinfection), and to keep cleaning and disinfection products out of the reach of children (see Method for cleaning and disinfection; fifth point). People who are more vulnerable to the effects of these products (e.g., people with asthma) may want to take additional protective measures such as avoiding the use of these products or only using them when necessary, staying in another room while the products are being used, and choosing the least risky products available (64). Following these guidelines can reduce the risks linked to virus exposure while preventing the risks associated with cleaning and disinfection products.
Method for cleaning and disinfection
- It is necessary to use paper towels or clean cloths for cleaning.
- As disinfectant is less effective on a soiled surface, clean the surface with water and soap or detergent to first eliminate any debris or stains (65,66); rinse with clean water and dry with a clean towel; apply the disinfectant as needed; then leave the disinfectant solution to act for a few minutes (according to the manufacturer’s instructions) before wiping off all traces of the product with a clean cloth. After disinfecting with a diluted water and bleach solution, rinse any surfaces that may come into contact with food or any object that may touch a person’s mouth or eyes (67). Start by cleaning the cleanest areas and finish with the dirtiest areas (68). All frequently touched surfaces must be cleaned regularly.
- Electronic devices, such as computer keyboards, tablets, and cell phones, can be disinfected with commercial pre-soaked alcohol wipes (at least once daily) or follow the manufacturer’s recommendations for cleaning and disinfection products suitable for the device.
- In indoor public spaces, frequently touched surfaces must be cleaned at least once daily and, if possible, more frequently depending on the intensity of their use (1,64,69). They must also been cleaned as soon as they are visibly dirty. Surface cleaning is particularly important in common areas like bathrooms and kitchens (1,52,66). It is not necessary to systematically disinfect after cleaning, except in specific situations (see the following point) (64,66,68,70). By eliminating dirt and impurities, cleaning is considered to eliminate 90% of the microorganisms present on surfaces (31,65–68). Cleaning is in fact considered the most important step of the complete pathogen elimination process (71).
- Disinfection must be carried out when an individual infected with COVID-19 or presenting symptoms compatible with the disease has stayed in the room (see Method for cleaning and disinfecting inanimate objects and surfaces in places where infected people have stayed) (64,68,70). Disinfectants with a drug identification number (DIN) are recommended for this purpose (1). Kampf et al. (2020) have demonstrated that bleach solutions (sodium hypochlorite diluted to 0.1% to 0.5%), ethanol (62% to 71%), and hydrogen peroxide (0.5%) were very effective for disinfecting surfaces contaminated with coronaviruses2(72). To prepare a bleach solution diluted to 0.1% using basic household bleach (with a 5% concentration), one part bleach is added to 50 parts water.3 This concentration is considered adequate for disinfecting hard (non-porous) surfaces. The minimum recommended contact time is one minute. This solution must be prepared daily and, as with all cleaning products and disinfectants, stored safely out of the reach of children.
- Environments that applied cleaning and disinfection procedures before the pandemic (e.g. slaughterhouses) must continue these procedures during this period.
- Shared objects and equipment must be reserved for a single group (organize objects and equipment by group of individuals) so that they can be cleaned only once daily. If it is not possible to reserve the equipment for a single group, it is suggested, as set out in the INSPQ document on daycare facilities (73) [in French only], that the equipment be cleaned between each group of users. This recommendation applies to daycare centres, schools, and workplaces, excluding healthcare settings.
- If possible, one should avoid using spray bottles (2,74) to limit aerosolization of disinfectants, which could be inhaled and irritate the airways and cause respiratory problems (2,62,74,75). However, if a spray bottle is used, adjust it to a spray setting with large droplets (74).
Appropriate protective measures for cleaning and disinfection
- Wear waterproof gloves for hand protection when cleaning (64).
- Hands must be washed before and after wearing gloves. Wash hands with water and soap (for at least 20 seconds) after removing gloves (76).
- Make sure to properly ventilate the room during cleaning and disinfection operations (64).
- After the cleaning and disinfection, carefully wash washable gloves with water and detergent and then dry them, or discard and replace the gloves with a new pair, as applicable.
- Once the cleaning and disinfection operations are complete, remove the non-disposable personal protective equipment used, if applicable, and wash it (74).
- Wear an RPD (respiratory protective device) when warranted and as specified in the product manufacturer’s instructions.
Method for cleaning and disinfecting inanimate objects and surfaces in places where infected people have stayed
- The cleaning procedures must be optimized in areas where infected people have stayed for hours at a time. It is suggested that the premises be cleaned and disinfected, especially objects and surfaces infected individuals have touched (77). The usual cleaning products and disinfectants may be used to carry out these tasks.
- “The available experimental and epidemiological data support aerosol transmission in close proximity (within 2 meters). The risk of SARS-CoV-2 transmission increases in closed, crowded and, inadequately ventilated spaces, and with prolonged exposure. The data have demonstrated that transmission by close contact remains the main transmission vector involved. However, they also suggest that aerosol transmission could occur at a distance. The maximum distance remains inexact, but it is unlikely to be more than a few meters” (78). At present, the scientific community cannot exactly determine the actual persistence time of the virus in open air (30,79). However, it has been observed in an experimental situation that the median half-life of SARS-CoV-2 in aerosols was approximately one hour (30). Also, considering that the recommendations in this document are mainly intended for residential, community, and work settings (excluding healthcare settings) where the clinical condition of the infected individual and ventilation situation of the premises are often unknown, disinfection measures are possibly less rigorous than in a healthcare setting, and there is often little or no personal protective equipment available, it is recommended to close, as much as possible, the areas used by infected individuals and to wait one hour (as a precaution) before starting cleaning and disinfection (80). If possible, optimize the fresh air intake by the mechanical ventilation system or open the windows to the outside to increase the air circulation in the area concerned. This waiting period will also help promote the gradual inactivation of the virus on surfaces.
- For hard and non-porous surfaces, the usual cleaning products and disinfectants can be used to carry out cleaning tasks. Allow the disinfectant to have sufficient contact time with the surfaces or objects to inactivate the virus (refer to the manufacturer’s specifications for this information).
- For porous surfaces such as carpets and curtains, eliminate any visible contamination, when present, while cleaning with products suitable for use on these surfaces. After cleaning, if the articles can be washed, wash them in accordance with the manufacturers’ instructions using the hottest water appropriate for these articles, if possible (1,56), and then dry them completely afterwards.
- Clothes and other articles that go in the laundry may be washed using the hottest water recommended for these articles, when possible (56). Take soiled linen (e.g., sheets, towels, clothes) to the laundry area in a cloth or plastic bag. Avoid shaking the laundry or the container while placing the laundry in the washing machine. Avoid contact between skin or clothing and the contaminated laundry. The laundry can however be washed with laundry from other members of the household or facility concerned, using a regular laundry detergent. However, if the clothes are heavily soiled (e.g., with vomit), they must be cleaned beforehand or even washed separately.
- The infected individual’s dishes and utensils can be washed after use in the usual manner with soap and water. Using a dishwasher is also acceptable.
- Tissues and disposable items used by the infected individual must be disposed of in a garbage bin equipped with a bag and ideally, a cover. Close the bag before disposing of it in the container used for regular garbage collection.
Cleaning and disinfection in outdoor environments
- As set out in the publication COVID-19: Outdoor environment (34), SARS‑CoV‑2 transmission via contaminated inanimate objects and surfaces (fomites) is considered possible despite limited epidemiological evidence. In outdoor environments, the presence of SARS‑CoV‑2 on objects and surfaces can be affected by various factors (sun radiation, wind, precipitation, temperature, humidity, etc.). “In order to reduce the risk of transmission via fomites, the various surfaces of street furniture can be cleaned in the usual manner and generally do not require disinfection” (34).
- Using disinfectant in aerosol form (spraying, fumigation) in outdoor spaces (e.g., streets, market squares) is not recommended in the context of COVID-19 (2,81). This method has not been proven effective at reducing the risk of infection and carries risks for the environment and the staff carrying out the work, as some products used can cause irritation to the airways (82).
- For cleaning operations related to indoor and outdoor recreational activities, refer to the guidelines and recommendations issued by recognized organizations (83-86).
Quarantining items shared between groups that cannot be cleaned or disinfected
- Sharing objects between groups should be limited as much as possible in the context of a pandemic, especially any objects that come in contact with a person’s face or head.
- If sharing objects between groups cannot be avoided, it may be recommended to remove or store (quarantine) shared materials that cannot be cleaned and disinfected (see Figure 1) (87).
- Some situations may or may not require a quarantine, either for all alert levels or only in red zones. The proposed recommendations for these various scenarios are described below (see Figure 1).
- A number of factors may influence these recommendations: the risk of infected persons, whether symptomatic or not, being present; the risk of contamination of objects by respiratory secretions (that is the main means of viral emission); the number of people potentially in contact with the object; vaccination status; and the ability to comply with recommended hygiene measures; to name a few.
- Under experimental conditions, the length of time that the virus remains cultivable varies depending on the material of the object or surface. Objects may also be made of more than one type of material. In order to account for the various types of materials on which the virus has a slightly longer half-life (e.g., plastic compared to paper or clothing), it is generally suggested that the minimum length of quarantine be 24 hours, where applicable (see below and Figure 1).
- For clothing used in fitting rooms in stores, a minimum quarantine period of three hours could be applied when appropriate (Figure 1). The short half-life of the virus on this material, the brief length of contact between the person and the fabric, and the protective effect of other hygiene measures applied (hand-washing before and after trying on clothes, mask wearing, regular cleaning of the fitting room) can justify this shorter quarantine period of three hours.
Figure 1 - Quarantine suggestions for objects shared between groups that cannot be cleaned or disinfected***, excluding healthcare settings
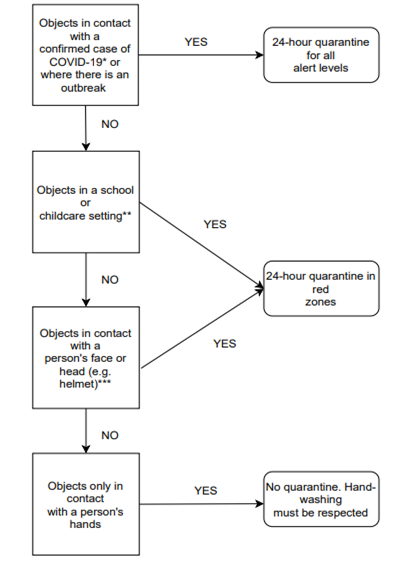
* For objects that have come in contact with a confirmed case of COVID-19, quarantine applies, regardless of whether or not they are shared between groups.
** Lending sports equipment in a childcare or school setting could be permitted if a person in charge can ensure that the children comply with hand-washing instructions before and after handling the equipment.
*** For clothing used in fitting rooms in stores, a minimum quarantine period of 3 hours could be applied.
Objects touched by a confirmed case of COVID-19 or where there is an outbreak, that cannot be cleaned and disinfected
Objects touched by a confirmed case of COVID-19 or where there is an outbreak and that cannot be cleaned and disinfected should be quarantined for a minimum of 24 hours, whatever the alert level for the region. An alternative could be to use a steam cleaner (according to the manufacturer’s recommendations, 5 minutes with 70°C steam and 1 minute with 100°C steam) (52). For articles of people deceased from COVID-19, see the INSPQ publication Preventive and Protective Measures for Funeral Services Businesses (88).
Objects in school or childcare environments that cannot be cleaned and disinfected and that are shared between groups
It would be preferable to continue to apply a minimum 24-hour quarantine in school and childcare settings in red zones, given the challenges of children’s compliance with hygiene measures, like hand-washing, as well as the ongoing uncertainty around the role of children in transmitting the infection (89). This quarantine does not apply to other alert levels. However, for sports equipment lent out in these settings, given the benefits of practicing sports activities for young people, if a person in charge can supervise the children’s hand-washing before and after handling the equipment, the equipment could be lent out without a quarantine, if a quarantine would be too restrictive due to, for example, the quantity of equipment available.
Objects that come in contact with a person’s face or head, that cannot be cleaned and disinfected, and that are shared between groups
For shared objects that come in contact with a person’s face or head, a minimum quarantine of 24 hours should be applied. It seems reasonable to only apply this measure in red zones, where community transmission is well established.
Objects that only come in contact with a person’s hands, that cannot be cleaned and disinfected, and that are shared between groups
For all objects made of any non-washable materials and that only come in contact with people’s hands in an environment in which only adults are present, it could be possible to not apply a quarantine, in any zone. It would then have to be possible to ensure that good hand hygiene practices are applied at all times.
Glossary
Aerosols: Aerosols are particles suspended in the air, whose movement is mainly governed by their size. They are generally smaller than 100 micrograms (µm) and are potentially inhalable. These particles have been typically called droplets when larger than 5 µm. They can be classified according to the anatomical site of the airway on which they are deposited:
- Nasopharyngeal particles, which are deposited in the nose or throat (≤ 100 µm)
- Tracheobronchial particles, which are deposited in the bronchi (≤ 15 µm)
- Alveolar particles, which reach the pulmonary alveoli (≤ 5 µm), typically called “microdroplets”
Cultivable: The quality of a virus being able to reproduce itself on appropriate cell cultures under the right conditions. A virus being cultivable does not necessarily mean that it is infectious.
Surface disinfection: Disinfection done using chemical products to destroy the microorganisms remaining on a surface after cleaning, which further reduces the risk of spreading infection (1).
Fomites: Inanimate surfaces and objects.
Surface cleaning: The elimination of dirt and impurities, including microorganisms. Cleaning alone does not kill microorganisms, but partly eliminating them reduces their quantity, and in turn, the risk of spreading infection (1,2).
Appendix 1 - Methodology brief literature review
- Cautionary note on institutional methodology: YES
- Clear statement of research question or review objectives: YES
- Documentary research strategy (multiple answers are acceptable):
- COVID-19 scientific monitoring: YES
- Use of targeted institutional COVID-19 scientific monitoring (e.g., CHSLDs): NO
- Use of institutional scientific monitoring of grey literature: YES
- Specify the type of scientific monitoring (e.g., general COVID-19, or prevention/promotion) for a and b, along with the monitoring period covered for all three : Environmental health scientific monitoring, from August 1 to November 30, 2020.
- Establish a specific documentary research strategy (retrospective): NO
- Other: YES.
- Specify: Grey literature research for positions of recognized organizations.
- Use of inclusion criteria: NO
- Use of preprints
- Indicate their inclusion or exclusion: YES
- Facilitated identification of preprints in document: NO
- Data extraction - Inclusion of evidence tables : NO
- Assessment of the quality or standard of evidence in articles or other documents included: NO (Note that such assessment is not essential for this type of rapid response)
- Peer review (list peer reviewers’ names and affiliations on the credits page for b, c, and d) (multiple answers are acceptable)
1 See Health Canada’s list of approved and safe products for COVID-19 (53).
2 Among the products recommended by Health Canada for disinfecting hard surfaces, the ethanol concentration varies from 60% to 80%, while the range for isopropanol is 60% to 75% (53).
3 0.1% disinfecting bleach solution: add 5 ml (1 teaspoon) of bleach with a 5% base concentration to 250 ml (1 cup) of water.
References
- Cleaning and disinfecting public spaces during COVID-19. Government of Canada. 2020. Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/cleaning-disinfecting-public-spaces.html
- Cleaning and disinfection of environmental surfaces in the context of COVID-19. World Health Organization. 2020. Available at: https://www.who.int/publications-detail/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19
- Ye G, Lin H, Chen L, Wang S, Zeng Z, Wang W, Zhang S, Rebmann T, Li Y, Pan Z, et al. Environmental contamination of SARS-CoV-2 in healthcare premises. J Infect. 2020 Apr 30;81(2).
- Wu S, Wang Y, Jin X, Tian J, Liu J, Mao, Y. Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease 2019. Am J Infect Control. 2020;10.
- Zhou J, Otter J, Price JR, Cimpeanu C, Garcia DM, Kinross J, Boshier P, Mason S, Bolt F, Holmes AH, et al. (2020). Investigating SARS-CoV-2 surface and air contamination in an acute healthcare setting during the peak of the COVID-19 pandemic in London. medRxiv [Online]. 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.05.24.20110346v1
- Ryu B-H, Cho Y, Cho O-H, Hong SI, Kim S, Lee S. Environmental contamination of SARS-CoV-2 during the COVID-19 outbreak in South Korea. Am J Infect Control. 2020 May 30;48(8):875‑9.
- Lei H, Ye F, Liu X, Huang Z, Ling S, Jiang Z, Cheng, J, Zanin M. SARS-CoV-2 environmental contamination associated with persistently infected COVID-19 patients. Influenza Other Respir Viruses. 2020;14(6):688‑99.
- Binder RA, Alarja NA, Robie ER, Kochek KE, Xiu L, Rocha-Melogno L, Abdelgadir A, Goli SV, Farrell AS, Coleman KK, et al. Environmental and Aerosolized SARS-CoV-2 Among Hospitalized COVID-19 Patients. J Infect Dis. 2020;222(11):1798‑806.
- Colaneri M, Seminari E, Novati S, Asperges E, Biscarini S, Piralla A, Percivalle E, Cassaniti I, Baldanti F, Bruno R, et al. Severe acute respiratory syndrome coronavirus 2 RNA contamination of inanimate surfaces and virus viability in a health care emergency unit. Clin Microbiol Infect [Online]. 2020 Aug 1;26(8). Available at: https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(20)30286-X/abstract
- D’Accolti M, Soffritti I, Passaro A, Zuliani G, Antonioli P, Mazzacane S, Manfredini R, Caselli E, et al. SARS-CoV-2 RNA contamination on surfaces of a COVID-19 ward in a hospital of Northern Italy: what risk of transmission? Eur Rev Med Pharmacol Sci. 2020;24(17):9202‑7.
- Ding Z, Qian H, Xu B, Huang Y, Miao T, Yen H-L, Xiao S, Cui L, Wu X, Shao W, et al. Toilets dominate environmental detection of severe acute respiratory syndrome coronavirus 2 in a hospital. Sci Total Environ [Online]. 2020 Aug 15;753. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0048969720352396?via%3Dihub
- Kim UJ, Lee SY, Lee JY, Lee A, Kim SE, Choi O-J, Lee JS, Kee S-J, Jang H-C. Air and Environmental Contamination Caused by COVID-19 Patients: a Multi-Center Study. J Korean Med Sci [Online]. 2020 Sept 21;35(37). Available at: https://doi.org/10.3346/jkms.2020.35.e332
- Moore G, Rickard H, Stevenson D, Bou PA, Pitman J, Crook A, Davies K, Spencer A, Burton C, Easterbrook L, et al. Detection of SARS-CoV-2 within the healthcare environment: a multicentre study conducted during the first wave of the COVID-19 outbreak in England. medRxiv [Online]. Cold Spring Harbor Laboratory Press. 2020 Sept 25. Available at: https://www.medrxiv.org/content/10.1101/2020.09.24.20191411v1
- Mouchtouri VA, Koureas M, Kyritsi M, Vontas A, Kourentis L, Sapounas S, Rigakos G, Petinaki E, Tsiodras S, Hadjichristodoulou C, et al. Environmental contamination of SARS-CoV-2 on surfaces, air-conditioner and ventilation systems. Int J Hyg Environ Health. 2020 Sept 1;230:113599.
- Nelson A, Kassimatis J, Estoque J, Yang C, McKee G, Bryce E, Hoang L, Daly P, Lysyshyn M, Hayden AS, et al. Environmental detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from medical equipment in long-term care facilities undergoing COVID-19 outbreaks. Am J Infect Control. 2020 July 6.
- Pasquarella C, Colucci ME, Bizzarro A, Veronesi L, Affanni P, Meschi T, Brianti E, Vitali P, Albertini R. Detection of SARS-CoV-2 on hospital surfaces. Acta Bio-Medica Atenei Parm. 2020 July 20;91(9-S):76‑8.
- Peyrony O, Ellouze S, Fontaine J-P, Thegat-Le Cam M, Salmona M, Feghoul L, Mahjoub N, Mercier-Delarue S, Gabassi A, Delaugerre C. Surfaces and equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the emergency department at a university hospital. Int J Hyg Environ Health. Sept 2020;230:113600.
- Razzini K, Castrica M, Menchetti L, Maggi L, Negroni L, Orfeo NV, Pizzoccheri A, Stocco M, Muttini S, Balzaretti CM. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy. Sci Total Environ. 2020 Nov 10;742:140540.
- Santarpia JL, Rivera DN, Herrera VL, Morwitzer MJ, Creager HM, Santarpia GW, Crown KK, Brett-Major DM, Schnaubelt ER, Broadhurst MJ, et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci Rep. Nature Publishing Group. 2020 July 29;10(1):12732.
- Tan L, Ma B, Lai X, Han L, Cao P, Zhang J, Fu J, Zhou Q, Wei S, Wang Z, et al. Air and surface contamination by SARS-CoV-2 virus in a tertiary hospital in Wuhan, China. Int J Infect Dis [Online]. 2020 July 27;99. Available at: https://www.ijidonline.com/article/S1201-9712(20)30571-3/fulltext
- Wan B, Zhang X, Luo D, Zhang T, Chen X, Yao Y, Zhao X, Lei L, Liu C, Zhao W, et al. On-site analysis of COVID-19 on the surfaces in wards. Sci Total Environ [Online]. 2020 Aug 18;753. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0048969720352876?via%3Dihub
- Wei L, Lin J, Duan X, Huang W, Lu X, Zhou J, Zong Z. Asymptomatic COVID-19 Patients Can Contaminate Their Surroundings: an Environment Sampling Study. mSphere [Online]. 2020 June 24;5(3). Available at: https://msphere.asm.org/content/5/3/e00442-20
- Suzuki M, Kamiya H, Okamoto K, Yamagishi T, Kakimoto K, Takeda M, Matsuyama S, Shirato K, Nao N, Hasegawa H, et al. Environmental sampling for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during a coronavirus disease (COVID-19) outbreak aboard a commercial cruise ship. medRxiv. 2020 Jan 1. Available at: https://www.medrxiv.org/content/10.1101/2020.05.02.20088567v1
- Döhla M, Wilbring G, Schulte B, Kümmerer BM, Diegmann C, Sib E, Richter E, Haag A, Englehart S, Eis-Hübinger AM, et al. SARS-CoV-2 in environmental samples of quarantined households. medRxiv [Online]. June 2020. Available at: http://medrxiv.org/lookup/doi/10.1101/2020.05.28.20114041
- Fernández-de-Mera IG, Rodríguez Del-Río FJ, Fuente J de la, Pérez-Sancho M, Hervás D, Moreno I, Domínguez M, Domínguez L, Gortázar C. Detection of environmental SARS-CoV-2 RNA in a high prevalence setting in Spain. Transbound Emerg Dis [Online]. 2020 Sept 7. Available at: https://onlinelibrary.wiley.com/doi/10.1111/tbed.13817
- Hu X, Xing Y, Ni W, Zhang F, Lu S, Wang Z, Gao R, Jiang F. Environmental contamination by SARS-CoV-2 of an imported case during incubation period. Sci Total Environ [Online]. 2020 Nov 10;742. Available at: http://www.sciencedirect.com/science/article/pii/S0048969720341425
- Jiang F-C, Jiang X-L, Wang Z-G, Meng Z-H, Shao S-F, Anderson BD, Ma M-J. Detection of Severe Acute Respiratory Syndrome Coronavirus 2 RNA on Surfaces in Quarantine Rooms. Emerg Infect Dis J [Online]. Sept 2020;26(9). Available at: https://wwwnc.cdc.gov/eid/article/26/9/20-1435_article
- Luo L, Liu D, Zhang H, Li Z, Zhen R, Zhang X, Xie H, Song W, Liu J, Huang Q, et al. Air and surface contamination in non-health care settings among 641 environmental specimens of 39 COVID-19 cases. PLoS Negl Trop Dis [Online]. 2020 Oct 9;14(10). Available at: https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008570
- Ong SWX, Lee PH, Tan YK, Ling LM, Ho BCH, Ng CG, Wang DL, Tan BH, Leo Y-S, Ng O-T, et al. Environmental contamination in a COVID-19 intensive care unit–What is the risk? Infect Control Hosp Epidemiol. 2020;1‑9.
- van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med [Online]. 2020. Available at: http://www.nejm.org/doi/10.1056/NEJMc2004973
- Chin AWH, Chu JTS, Perera MRA, Hui KPY, Yen H-L, Chan MCW, Peiris M, Poon LLM. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe [Online]. 2020;1(1). Available at: http://www.sciencedirect.com/science/article/pii/S2666524720300033
- Harbourt D, Haddow A, Piper A, Bloomfield H, Kearney B, Gibson K, Minogue T. Modeling the Stability of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) on Skin, Currency, and Clothing. medRxiv [Online]. Cold Spring Harbor Laboratory Press. 2020 July 3. Available at: https://www.medrxiv.org/content/10.1101/2020.07.01.20144253v1
- Liu Y, Li T, Deng Y, Liu S, Zhang D, Li H, Wang X, Jia L, Han J, Bei Z, et al. Stability of SARS-CoV-2 on environmental surfaces and in human excreta. J Hosp Infect [Online]. 2020 Nov 1. Available at: http://www.sciencedirect.com/science/article/pii/S0195670120305041
- Comité santé environnementale de COVID-19. COVID-19: Outdoor environment. Institut national de santé publique du Québec. May 2020. Available at: https://www.inspq.qc.ca/en/publications/3002-outdoor-environment-covid19
- Schuit M, Ratnesar-Shumate S, Yolitz J, Williams G, Weaver W, Green B, Miller D, Krause M, Beck K, Wood S, et al. Airborne SARS-CoV-2 is Rapidly Inactivated by Simulated Sunlight. J Infect Dis. 2020 June 11;222(4):564‑71.
- Heilingloh CS, Aufderhorst UW, Schipper L, Dittmer U, Witzke O, Yang D, Zheng X, Sutter K, Trilling M, Alt M, et al. Susceptibility of SARS-CoV-2 to UV irradiation. Am J Infect Control. Elsevier. 2020 Oct 4;48(10):1273‑5.
- Brlek A, Vidović Š, Vuzem S, Turk K, Simonović Z. Possible indirect transmission of COVID-19 at a squash court, Slovenia, March 2020: case report. Epidemiol Infect [Online]. 2020 June 19;148. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7327185/
- Cai J, Sun W, Huang J, Gamber M, Wu J, He G. Early Release - Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg Infect Dis J [Online]. 2020;26(6). Available at: https://wwwnc.cdc.gov/eid/article/26/6/20-0412_article
- Xie C, Zhao H, Li K, Zhang Z, Lu X, Peng H, Wang D, CHen J, Zhang X, Wu D, Gu Y. The evidence of indirect transmission of SARS-CoV-2 reported in Guangzhou, China. BMC Public Health. 2020 Aug 5;20(1):1202.
- COVID-19 Transmission in Condo or Apartment Buildings Rapid Review. Alberta Health Services. 2020. Available at: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-sag-transmission-in-condo-or-apartment-buildings-rapid-review.pdf
- Pung R, Chiew CJ, Young BE, Chin S, Chen MI-C, Clapham HE, Cook AR, Maurer-Stroh S, Toh MPHS, Poh C et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. The Lancet. 2020 Mar 28;395(10229):1039‑46.
- Sia SF, Yan L-M, Chin AWH, Fung K, Choy K-T, Wong AYL, Kaewpreedee, P, Perera RAPM, Poon LLM, Nicholls JM, et al. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature. July 2020;583(7818):834‑8.
- Brurberg, KG. Transmission of SARS-CoV-2 via contact and droplets, 1st update – a rapid review. Norwegian Institute of Public Health. 2020. Available at: https://www.fhi.no/en/publ/2020/Transmission-of-SARS-CoV-2-via-contact-and-droplets-1st-updat-/
- COVID-19 Routes of Transmission – What We Know So Far. Public Health Ontario. 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/wwksf-routes-transmission-mar-06-2020.pdf?la=en
- Transmission of SARS-CoV-2: implications for infection prevention precautions. World Health Organization. 2020. Available at: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions
- Dietz L, Horve PF, Coil DA, Fretz M, Eisen JA, Wymelenberg KVD. 2019 Novel Coronavirus (COVID-19) Pandemic: Built Environment Considerations To Reduce Transmission. mSystems [Online]. 2020 Apr 28;5(2). Available at: https://msystems.asm.org/content/5/2/e00245-20
- Kampf, Brüggemann Y, Kaba HEJ, Steinmann J, Pfaender S, Scheithauer S, Steinmann E. Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2. J Hosp Infect [Online]. 2020 Sept 18. Available at: https://www.journalofhospitalinfection.com/article/S0195-6701(20)30437-0/abstract
- Kanamori H, Weber DJ, Rutala WA. The role of the healthcare surface environment in SARS-CoV-2 transmission and potential control measures. Clin Infect Dis [Online]. 2020. Available at: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1467/5912347
- Karia R, Gupta I, Khandait H, Yadav A, Yadav A. COVID-19 and its Modes of Transmission. SN Compr Clin Med. 2020 Sept 1;1‑4.
- Vella F, Senia P, Ceccarelli M, Vitale E, Maltezou H, Taibi R, Lleshi A, Venanzi Rullo E, Pellicanò GF, Rapisarda V, et al. Transmission mode associated with coronavirus disease 2019: a review. Eur Rev Med Pharmacol Sci. July 2020;24(14):7889‑904.
- How COVID-19 Spreads. Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html
- COVID-19: cleaning in non-healthcare settings outside the home. Public Health England. Government of the United Kingdom. Oct 2020. Available at: https://www.gov.uk/government/publications/covid-19-decontamination-in-non-healthcare-settings
- Hard-surface disinfectants and hand sanitizers (COVID-19). 2020. Health Canada. Government of Canada. Available at: https://www.canada.ca/fr/sante-canada/services/medicaments-produits-sante/desinfectants/covid-19.html
- Expedited access to disinfectants, hand sanitizers and personal protective equipment to help limit the spread of COVID-19, as well as swabs for testing. Health Canada. Government of Canada. 2020. Available at: https://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2020/72623a-eng.php
- Coronavirus Disease 2019 (COVID-19) Cleaning and Disinfection for Public Settings. Public Health Ontario. 2020. Available at: https://www.publichealthontario.ca/-/media/documents/ncov/factsheet-covid-19-environmental-cleaning.pdf?la=fr
- Cleaning and Disinfecting Your Home: Every Day and When Someone is Sick. Centers for Disease Control and Prevention. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/disinfecting-your-home.html
- Increases in exposure calls related to selected cleaners and disinfectants at the onset of the COVID-19 pandemic: data from Canadian poison centres. Public Health Agency of Canada. Government of Canada. 2020. Available at: https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-41-no-1-2021/exposure-cleaners-disinfectants-covid-19-pandemic-canadian-poison-centres.html
- Chang A, Schnall AH, Law R, Bronstein AC, Marraffa JM, Spiller HA, Hays HL, Funk AR, Mercurio-Zappala M, Calello DP, et al.. Cleaning and Disinfectant Chemical Exposures and Temporal Associations with COVID-19 — National Poison Data System, United States, January 1, 2020–March 31, 2020. MMWR Morb Mortal Wkly Rep [Online]. 2020;69(16):496-8. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6916e1.htm
- Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, Berling K, Mercante JW, Murphy JL, Garcia-Williams AG. Knowledge and Practices Regarding Safe Household Cleaning and Disinfection for COVID-19 Prevention — United States, May 2020. MMWR Morb Mortal Wkly Rep [Online]. 2020;69(23);705-9. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6923e2.htm
- A Rapid Review of Disinfectant Chemical Exposures and Health Effects During COVID-19 Pandemic. National Collaborating Centre for Environmental Health. Oct 2020. Available at: https://ncceh.ca/documents/field-inquiry/rapid-review-disinfectant-chemical-exposures-and-health-effects-during
- Folletti I, Zock J-P, Moscato G, Siracusa A. Asthma and rhinitis in cleaning workers: a systematic review of epidemiological studies. J Asthma Off J Assoc Care Asthma. Feb 2014;51(1):18‑28.
- Zock J-P, Plana E, Jarvis D, Antó JM, Kromhout H, Kennedy SM, Künzli N, Villani S, Olivieri M, Torén K, et al. The use of household cleaning sprays and adult asthma: an international longitudinal study. Am J Respir Crit Care Med. 2007 Oct 15;176(8):735‑41.
- Moual NL, Varraso R, Siroux V, Dumas O, Nadif R, Pin I, Zock J-P, Kauffmann F. Domestic use of cleaning sprays and asthma activity in females. Eur Respir J. 2012 Dec 1;40(6):1381‑9.
- Cleaning Your Facility: Every Day and When Someone is Sick. Centers for Disease Control and Prevention. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/reopen-guidance.html
- COVID-19 Public Health Recommendations for Environmental Cleaning of Public Facilities. Alberta Health Services. 2020. Available at: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-environmental-cleaning-public-facilities.pdf
- Cleaning for COVID-19 - advice for sectors outside the healthcare service. Norwegian Institute of Public Health. 2020. Available at: https://www.fhi.no/en/op/novel-coronavirus-facts-advice/advice-and-information-to-other-sectors-and-occupational-groups/cleaning-and-disinfection/
- Pratiques de base - Entretien, hygiène et salubrité des objets, des surfaces et des locaux. In: Prévention et contrôle des infections dans les services de garde et écoles du Québec - Guide d’intervention. Ministère de la Santé et des Services sociaux. Gouvernement du Québec. 2019. p. 53‑69. Available at: https://publications.msss.gouv.qc.ca/msss/fichiers/guide-garderie/chap4-entretien-hygiene.pdf
- Cleaning Guidelines for the Prevention of COVID-19 Infections. Finnish Institute of Occupational Health. 2020. Available at: https://www.ttl.fi/en/cleaning-guidelines-for-the-prevention-of-covid-19-infections
- Individual and community-based measures to mitigate the spread of COVID-19 in Canada. Government of Canada. 2020. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-cor…
- Cleaning and Disinfecting: Best Practices During the COVID-19 Pandemic. United States Environmental Protection Agency. 2021. Available at: https://www.epa.gov/coronavirus/cleaning-and-disinfecting-best-practices-during-covid-19-pandemic
- Center for Food Security and Public Health. Disinfection 101. Iowa State University. May 2008. Available at: http://www.cfsph.iastate.edu/Disinfection/Assets/Disinfection101.pdf
- Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246‑51.
- SAT-COVID-19 Working Group. Services de garde en installation : Mesures de prévention de la COVID-19 en milieu de travail - Recommandations intérimaires. Institut national de santé publique du Québec. Aug 2020. Available at: /sites/default/files/covid/2984-travailleuses-services-garde-covid19.pdf
- Coronavirus SARS-CoV-2 : nettoyage et désinfection des établissements recevant du public et des lieux de travail. Haut Conseil de la santé publique. 2020. Available at: https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=811
- Quirce S, Barranco P. Cleaning agents and asthma. J Investig Allergol Clin Immunol. 2010;20(7):542‑50.
- SAT-COVID-19 Working Group. COVID-19: Hierarchy of Control Measures in the Workplace - Preventive Measures in the Workplace. Institut national de santé publique du Québec. 2020. Available at: https://www.inspq.qc.ca/en/publications/3022-hierarchy-control-measures-workplace-covid19
- SAT-COVID-19 Working Group. Schools and teaching environments - COVID-19 Preventive Measures in the Workplace. Institut national de santé publique du Québec. 2020. Available at: https://www.inspq.qc.ca/en/publications/3056-schools-and-teaching-environments-covid19
- Anctil G, Caron S, Charest J, Irace-Cima A, Gilca V, Sauvageau C, Villeneuve j, Huot C, Lévesque B, Perron S. Transmission du SRAS-CoV-2 : constats et proposition de terminologie. Institut national de santé publique du Québec. 2021. Available at: https://www.inspq.qc.ca/publications/3099-transmission-sras-cov-2-constats-terminologie-covid19
- Fears AC, Klimstra WB, Duprex P, Hartman A, Weaver SC, Plante KS, Mirchandani D, Plante JA, Aguilar PV, Fernández D, et al. Persistence of Severe Acute Respiratory Syndrome Coronavirus 2 in Aerosol Suspensions. Emerg Infect Dis J [Online]. 2020;26(9). Available at: https://wwwnc.cdc.gov/eid/article/26/9/20-1806_article
- Scientific Brief: SARS-CoV-2 Transmission. Centers for Disease Control and Prevention. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html
- Can I use fogging, fumigation, or electrostatic spraying or drones to help control COVID-19? United States Environmental Protection Agency. United States government, 2020. Available at: https://www.epa.gov/coronavirus/can-i-use-fogging-fumigation-or-electrostatic-spraying-or-drones-help-control-covid-19
- COVID-19 in indoor environments — Air and surface disinfection measures. National Collaborating Centre for Environmental Health. 2020. Available at: https://ncceh.ca/documents/guide/covid-19-indoor-environments-air-and-surface-disinfection-measures
- Guide de normes sanitaires en milieu de travail pour le secteur des activités intérieures et extérieures de sport, de loisir et de plein air – COVID-19 – La SST, c’est l’affaire de tous! Commission des normes, de l’équité, de la santé et de la sécurité du travail. Gouvernement du Québec.2020. Available at: https://www.cnesst.gouv.qc.ca/sites/default/files/documents/dc100-2161-guide-sports-loisirs_0.pdf
- Guidelines specific to recreation and sports. Gouvernement du Québec. 2020. Available at: https://www.quebec.ca/en/tourism-and-recreation/sporting-and-outdoor-activities/resumption-outdoor-recreational-sports-leisure-activities
- Reducing COVID-19 risk in community settings: A tool for operators. Government of Canada. 2020. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/risk-mitigation-tool-outdoor-recreation-spaces-activities-operating-covid-19.html
- Huppé V, Huot C. Lieux de baignade. Institut national de santé publique du Québec. 2020. Available at: https://www.inspq.qc.ca/publications/3004-lieux-baignade-qr-covid19
- Guidance for Cleaning and Disinfecting Public Spaces, Workplaces, Businesses, Schools, and Homes. United States government. United States Environmental Protection Agency and Centers for Disease Control and Prevention. Apr 2020. Available at: https://www.epa.gov/sites/production/files/2020-04/documents/316485-c_reopeningamerica_guidance_4.19_6pm.pdf
- Côté R, Roy L-A, Valiquette L. COVID-19: Preventive and Protective Measures for Funeral Services Businesses. Institut national de santé publique du Québec. July 2020. Available at: /sites/default/files/publications/2913-funeral-services-businesses-covid19.pdf
- Comité sur les mesures populationnelles. Revue rapide de la littérature scientifique et données épidémiologiques provinciales de la COVID-19 parmi les jeunes âgés de moins de 18 ans. Institut national de santé publique du Québec. Dec 2020. Available at: /sites/default/files/covid/3007-enfants-risques-infections-transmission-covid19.pdf
AUTHOR
Caroline Huot, Public Health Medical Specialist
Comité en santé environnementale COVID-19 [COVID-19 Environmental Health Committee]
Direction de la santé environnementale et de la toxicologie
CONTRIBUTORS
Stéphane Perron, Public Health Medical Specialist
Stéphanie Potvin, Scientific Advisor
Comité en santé environnementale COVID-19 [COVID-19 Environmental Health Committee]
Direction de la santé environnementale et de la toxicologie
REVIEWERS
Stéphane Caron, Medical Advisor
COVID-19 Working Group
Direction des risques biologiques et de la santé au travail of the INSPQ
Geneviève Anctil, Nursing Advisor
Jasmin Villeneuve, Medical Advisor
Chantal Richard, Nursing Advisor
Comité prévention et contrôle des infections [Infection Prevention and Control Committee]
Direction des risques biologiques et de la santé au travail